#Industry News
Switch to PCR Stool Tests Reduces Health Care Use
A change to stool testing using multiplex polymerase chain reaction (PCR) technology was associated with reductions in endoscopy, abdominal radiology and use of antibiotics, according to the authors of a new study.
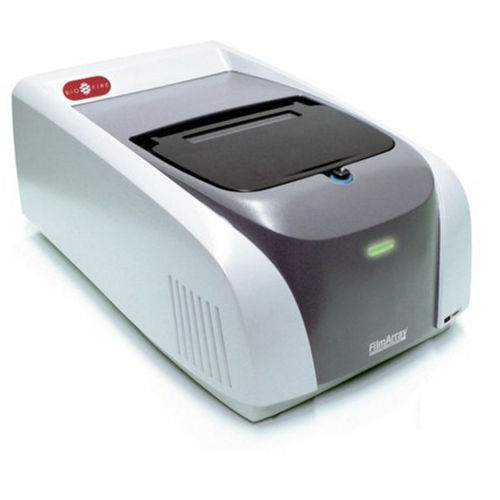
The researchers, from Columbia University Medical Center and NYU Langone Health, both in New York City, performed a retrospective analysis of patients at NewYork-Presbyterian/Columbia in New York City. In 2015, the health care system switched from stool culture and ova and parasites examination to the BioFire Diagnostics FilmArray GI panel to diagnose acute gastroenteritis. According to BioFire, the panel is able to detect 13 types of bacteria, four parasites and five viruses in little more than an hour.
The researchers compared use of health care resources between 9,402 patients tested for gastroenteritis with the FilmArray GI panel and 5,986 patients who received conventional stool culturing before the switch.
“Within 30 days following stool testing … patients who received a GI panel were less likely to undergo any endoscopic procedure (8.4% GI panel vs 9.6% stool culture, P=0.008) or any abdominal radiology (29.4% GI panel vs 31.7%, P=0.002),” the authors wrote. “Within 14 days following stool testing, patients who received a GI panel were less likely to be prescribed any antibiotic (36.2% GI panel vs 40.9%, P<0.001).”
“Even though [the FilmArray GI panel] is FDA approved, we really don’t know how it impacts patient management and clinical outcomes,” said Jordan Axelrad, MD, MPH, the study’s first author, whose group published its findings in the Journal of Clinical Microbiology (2019;26;56[1].pii: e01457-17). “This was an attempt to understand how the test is being utilized and how it impacts downstream health care utilization,” said Dr. Axelrad, of the Inflammatory Bowel Disease Center at NYU Langone Health.
“What they did that’s important is they took a systems-based view,” said Gary Procop, MD, the director of molecular microbiology, virology, mycology and parasitology at the Cleveland Clinic in Ohio. “They’re implementing a more expensive test, but demonstrating how it’s having a broader impact on patient care and decreasing overall health care delivery costs. This is critical, as we work to determine ways to implement these more expensive tests.”
The results were similar to a 2017 study, also published in the Journal of Clinical Microbiology, that also found the FilmArray GI panel was associated with lower health care costs and reductions in endoscopy, radiology and use of antibiotics, Dr. Axelrad said. The new study, however, did not find a reduced hospital length of stay nor a reduction in patients admitted, as did the previous research.
Both studies included disclosures of connections to BioFire, the company that makes the FilmArray tests. BioFire funded the 2017 study with an unrestricted grant; Dr. Axelrad said he did not receive funding but does consult for the company, including helping it produce a clinical guideline for the interpretation of the tests.
Dr. Axelrad added that the effect sizes were confounded by the fact that the group that underwent PCR testing had more hospitalized patients. “They were probably a sicker group of patients,” he said. “They tend to have more health care utilization at baseline.” Still, the analysis showed a drop in use, “so it likely underestimates the real impact.”
Dr. Procop said some people have voiced concern about FilmArray GI and similar tests because they detect organisms, such as viruses, that lack an associated treatment. Payors have denied coverage for the tests on that basis, he added.
These tests can still provide value, even when pathogens without a specific treatment are detected, Dr. Procop said, because they allow physicians to stop pursuing a diagnosis and order more tests or start a patient on unnecessary antibiotics.
“Overall, the cost to the health care system goes down when we use these broader panels,” he said. “But unfortunately, the payors, I just don’t think they see it, which is a real travesty.”
Dr. Axelrad said his team did not calculate the cost-effectiveness of the GI panel in terms of dollars saved. “It’s likely, given the improvements in utilization, we’d see a decrease in health care costs. But studies would be needed to delineate those cost savings.”