#Industry News
MAINTAINING QUALITY AND ENVIRONMENTAL STATE-OF-CONTROL
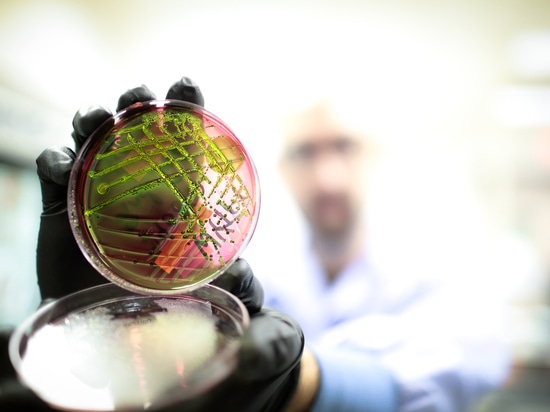
Environmental Monitoring and Accurate Organism Identification for medical device manufacturers; requirements, not suggestions
Medical Device Industry experts and Microbiology Consultants Melissa Stappen and Steve Langille with ValSource answer some frequently asked questions about medical device manufacturing, terminal sterilization and aseptic processes related to regulators expectations for maintaining control of manufacturing facilities and sending sterile and safe products to market.
Rachael: What are the main concerns currently impacting medical device manufacturers?
ValSource: There currently seems to be much confusion over how medical device manufacturers should be maintaining their environmental monitoring (EM) programs, how much monitoring is required and when and what to make of the results or subsequent microbiology testing required. Many medical device manufacturers running overkill sterilization cycles are uncertain about the requirements and recommendations pertaining to EM and microbiology testing. They feel because the overkill cycles are so robust, why would they need to do EM if everything is going to be killed on that device when exposed to the cycle?
The important fact here is the need for a solid EM program and quality assurance testing, in order to maintain a sanitary production environment. Providing data that your production environment is sanitary means you are producing quality products in a controlled environment. Processes and data; samples obtained during the EM program; having set metrics for alert and action limits; and providing microbiology testing data, bioburden, microbial identification, and endotoxin testing provide proof that you know your facility, you understand and track your environment, and are producing products in a state-of-control. FDA-regulated companies are required to build quality management systems and develop limits and alerts that allow for corrective actions to mitigate risk and address regulatory compliance observations with effective strategies that can be interpreted and communicated to avoid any data breaches causing regulatory bodies to take action.
Many believe just knowing they have organisms is good enough, but that is not the case. You cannot have full control and ability to mitigate risk unless you know what types of organisms your facility has. You need to understand the organism’s identity to know if it could affect product quality, then develop effective cleaning and sanitation protocols to mitigate the risk to the product. Tracking and understanding root cause of the organisms is also required and can only be determined by recording all organism identifications. Providing manufacturing facility environmental monitoring data and organism identification during an audit will provide concrete proof that you are in control of your facility. If you are unable to provide this data, it might be assumed that you are producing products in a non-sanitary environment and releasing products that are a risk to patients.
Rachael: How is a sterilization process validated?
ValSource: Process qualification and validation will vary depending upon the sterilization process. Following initial validation, terminal sterilization is typically re-qualified every year or two. Validation of terminal sterilization processes often uses chemical or biological indicators in the process to prove sterilization is working. Validation of aseptic processing is much more difficult and usually entails media fills and aseptic processing simulations conducted every six months, or more often if product fill lines are being changed. Medical device sterilization validation and re-qualification protocols are created and driven by the medical device firm that is instituting these processes.
Environmental monitoring and microbiology testing, specifically identifications, should be performed regularly. You need control of the environment. It is not a regulatory mandate, but it is in the manufacturer’s best interest to be able to demonstrate control by providing information regarding suspect organisms, personnel, flow, sanitization practices, or seasonal shifts in the microbiological flora on the manufacturing floor. If you do not have proof of manufacturing conditions, you could be issued 483 observations stating you lack control of the environment. Action and alert limits are established by the manufacturer, and the monitoring of viable and nonviable particulate matter will ensure you are managing your facility correctly.
In addition to knowing the number of microorganisms in the manufacturing area, it’s also important to identify the organisms, preferably to the species level, to know how to properly clean and sanitize the environment. If you don’t know what you have, you have no way of knowing how to mitigate it.
Rachael: Have you experienced or are you aware of any known sterility or endotoxin failures post-sterilization?
ValSource: First let us clarify that endotoxin is not at all affected by most sterilization processes. Sterilization processes destroy viable organisms but usually do not mitigate or destroy endotoxin. A product needs to be free of endotoxin prior to the sterilization process. Depyrogenation measures are in-process methods to aseptically provide components and/or solutions free of endotoxin, to your finished product. If a direct depyrogenation process to your finished product cannot occur due to the nature of the product, aseptic processes need to be in place to negate endotoxin levels. We have seen endotoxin failures in medical device products; however, these issues usually occur after product release and are not very common. Bacterial endotoxin contamination is managed during in-process testing and typically any endotoxin present in the product is detected before the product is sent out to the public.
Regarding sterility, yes, there have been post-sterilization failures of medical devices. These are usually due to container or packaging leaks, sterilization equipment failures, or incorrect calculation of the dose of sterilant. The industry sometimes tends to blend sterility and endotoxin control; although related because they both are associated with microbiological contamination, they should each be controlled on their own separate platforms.