#Industry News
Omicron virus antigenic detection brings great challenges in speed and sensitivity
Omicron virus antigenic detection brings great challenges in speed and sensitivity
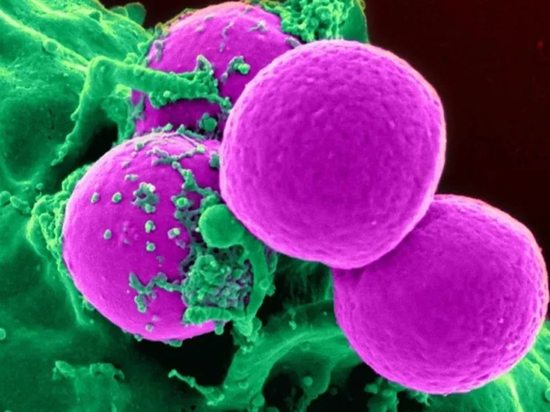
The detection of the detection rate of medRxiv is a major challenge in terms of speed and sensitivity. According to preliminary data from the medRxiv, the sensitivity of COVID-19's allergy virus to the existing rapid antigen detection challenges, but the data are still uncertain.
The sensitivity of antigen detection is a problem. It seems that the faster infection process of mutant strains may undermine the effectiveness of rapid detection, which is another problem, especially the self-test carried out by individuals before important activities.
According to a notice issued by the U.S. Food and Drug Administration FDA at the end of February, early studies led by the Radx project of the National Institutes of health showed that the sensitivity of rapid antigen detection to Omicron variants was reduced.
However, this is a very small number of people who are responsible for the analysis of the project, and Bruce is not the final conclusion.
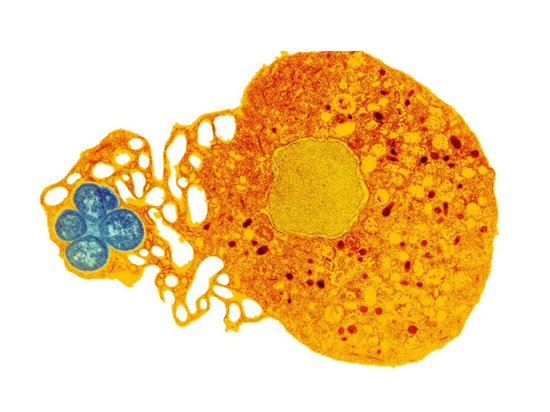
The data released by FDA comes from Radx researchers at Emory University. They obtained nine omicon samples from the University of Washington cooperative laboratory. They used these samples to create a series of diluents, and then carried out various rapid antigen tests and PCR tests. They also tested the delta variant and the wild-type virus.
In the three test cells they made, they can dilute more in the delta cell than in the Omicron cell. Compared with Omicron, in the case of delta variation, rapid antigen tests can detect delta virus at a higher PCR cycle threshold, which further indicates that these tests are more sensitive to delta.
Tromberg said that although this dilution experiment is the first step to evaluate whether and how Omicron affects the performance of rapid testing, the gold standard is to go into the clinic, measure the actual patients, and pay attention to when samples are collected after symptoms appear, and whether patients are vaccinated and enhanced before infection, because all these are important.
Does a decrease in laboratory test sensitivity mean a decrease in clinical sensitivity? This is still an outstanding issue.
Tromberg said that this work is ongoing, but he noted that the clinical data collected so far found that rapid detection actually performed better in actual clinical samples than in mixed series dilutions.
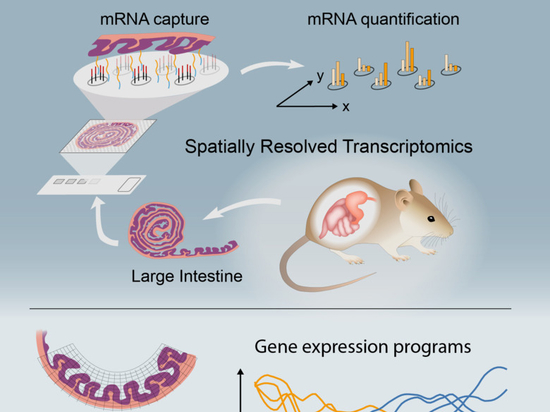
He acknowledges that this is an counterintuitive result, but believes that it may reflect differences in the time points at which different samples were collected during infection. Previous studies have observed that the ratio of N protein to nucleic acid collected from swab samples will change during infection. This means that the relationship between N protein concentration and pcr-ct values will vary depending on the sampling time during infection. He said that during the infection process, the difference between the collection time of experimental samples and clinical samples may drive the apparent sensitivity data. Omicron infects individuals significantly faster and more efficiently, which may mean that people should be tested earlier than previous strains after exposure.
He mentioned a Radx funded study from the University of Illinois that looked at the effectiveness of rapid antigen testing compared to PCR in the early environment of omicon. The study showed that the window period for rapid antigen detection of infection was about 3 to 6 days.
"This is a fairly wide window. What we are considering is to compress the detection window of Omicron." He said. "The attack rate of this virus is very high, and the best time is shortened. Therefore, I recommend that people test within one or two days of known or suspected infection."
In the medrxiv preview report of 2019 coronavirus disease released last week, researchers from the cvid-19 movement and social work group found the difference between rapid antigen detection and PCR in a group of 30 individuals in December 2021.
By observing these 30 individuals (29 of whom showed S gene deletion associated with Omicron variant), the study found that in all cases, the day and the second day of PCR detection of the first positive, rapid antigen detection produced false negative results.
During this period, the pcr-ct value of 28 of them was lower than 29, indicating that the viral load was higher than the infectivity threshold. On the second day after the initial positive PCR test, 75% of the individuals were still negative through the rapid antigen test, while on the third day, more than 80% of the subjects were positive for the rapid antigen test, and on the fourth day, 100% of the subjects were positive for the rapid antigen test.
The researchers also found four cases of transmission when a person was negative for the virus by rapid antigen testing. The study used Abbott's binaxnow and quidel's quickvue test.
The University of Illinois study also observed that rapid antigen detection did not detect early infection like PCR.
"If you line up the sensitivity of antigen detection and salivary RT-PCR a few days before the first infection is positive, the sensitivity of salivary PCR is very high, such as 80%, and the sensitivity of antigen is as high as 30%," he said. "You see the difference between these two methods. So it's not strange."
A paper published in the new England Journal of medicine last week also highlighted the fact that no matter what kind of COVID-19 mutation is involved, rapid antigen detection products will miss many patients on the first day of infection.
Blythe Adamson, the first author of medrxiv research, said that in her work, she found that the effectiveness of PCR and rapid antigen detection has decreased. This decline is not necessarily due to the decline in the performance of the detection itself, but due to the rapid infection of individuals by Omicron, which reduces the effectiveness of antigenic detection for individuals before the transmission of the virus.
"For Omicron, someone will detect a false negative, and we will find the infection (transmitted by seemingly negative individuals) after 12 to 24 hours, which is much faster than what we see in any other variant," Adamson said
"Because of this, I began to worry that the rigorous testing and security protocols we have been using may no longer be sufficient to meet the needs of Omicron," she said. "Therefore, for a period of time in these workplaces, not for research purposes, but for safety purposes, we have added daily antigen detection to daily PCR detection."
The emergence of Omicron raises the question of how useful rapid antigen testing is to determine whether individuals can safely participate in important activities without worrying about infection or transmission of the virus.
"When we try to screen people for high-risk activities, we have to be very careful. If they have no symptoms, rapid antigen testing may not be a good tool to make sure someone is negative and non infectious before attending a party," she said
Tromberg said he believes these tests are still useful, but recommends regular and continuous use rather than spot checks before meetings or events.
Overall, the effectiveness of rapid antigen detection in preventing COVID-19 from spreading at population level has been proved very little. Some observers attribute this to a lack of good methods for using such tests.