#Product Trends
SpaceGen‘s Genotyping Research in Ovarian Endometrioid Carcinoma
Study on genotyping application in ovarian endometrioid carcinoma.
Abstract
Ovarian endometrioid (ENOC) is one of the important subtypes of ovarian cancer, accounting for 10-15.8%, which is related to endometriosis and Lynch syndrome. The morphological heterogeneity of ENOC is high, and the prognosis is also different. ENOC and endometrioid carcinoma (EEC) have many similarities in molecular characteristics and histology. The application of molecular typing in endometrial cancer has become increasingly mature, and it also has some application exploration in ovarian cancer and primary double cancer of endometrium and ovary.
Background
Ovarian cancer ranks eighth in the number of new cases and deaths among women in the world, and tenth in the number of new cases and ninth in the number of deaths among Chinese women. In 2020, there will be 55342 new cases of ovarian cancer in China, with 37519 deaths, which is one of the main causes of death of gynecological cancer patients.
Epithelial ovarian cancer (EOC) is the most common type of ovarian cancer, which can be divided into high-grade serous cancer (HGSOC), low-grade serous cancer (LGSOC), ENOC, clear cell cancer (OCCC), mucinous cancer (MOC), etc. ENOC accounts for 10-15.8% of EOC. Compared with HGSOC, women with ENOC are on average 6 years younger (more commonly premenopausal), and about a quarter of ENOC are accompanied by synchronous endometrial cancer. It is estimated that 84~95% of ENOC cases are G1 and G2, and G3 accounts for 5~16%.Although more than 70% of ENOC patients are in early stage (FIGO I/II), the prognosis of some ENOC patients is still poor.
ENOC has high morphological heterogeneity, and common molecular changes affect WNT/β-Catenin pathway (CTNNB1 mutation, 53%), PI3K pathway (PIK3CA, 40%; PTEN, 17%), MAPK pathway (KRAS, 33%), and SWI/SNF complex (ARID1A, 30%).
Pathogenesis
Endometriosis: About 25-80% of ENOC patients also have endometriosis. Compared with healthy women without endometriosis, the risk of ENOC in patients with endometriosis is 2.32 times higher.
Hereditary tumor: about 7%~18% of ENOC have dMMR, which may be related to Lynch syndrome. BRCA1/2 gene mutation is not common in ENOC.
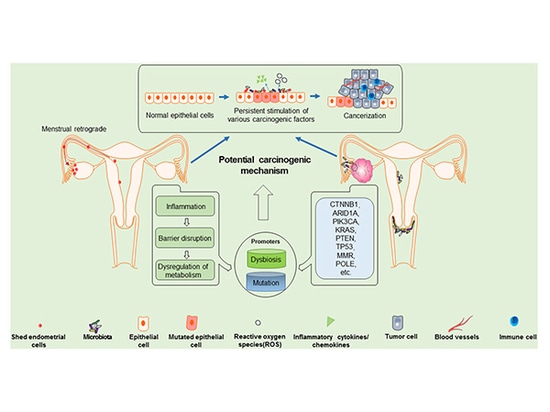
In recent years, the ecological imbalance of the microbiota in the female reproductive tract is considered to be related to the pathogenesis of endometrial cancer and ovarian cancer, and some specific carcinogenic pathogens have been found to contribute to the development of cancer. It has been shown that the imbalance of microenvironment and the accumulation of mutations are the stimulators for the progression of endometrioid ovarian cancer.
Potential carcinogenic mechanism of ENOC: exfoliated endometrial cells may migrate retrogradely to the ovary, which may be a promoting factor of ENOC. With the ecological imbalance of microenvironment and the accumulation of mutation load, the exfoliated endometrial cells and ovarian epithelial cells may gradually evolve into atypical cells, and further transform into cancer.
Treatment plan
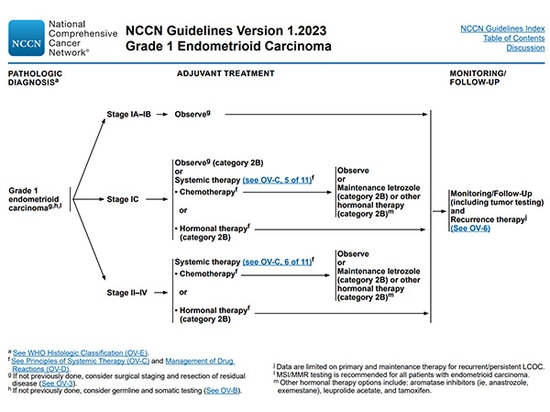
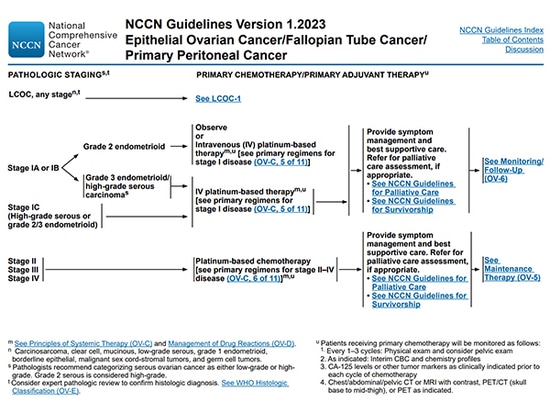
For G1 patients, observation is encouraged for patients in IA/IB stage. Patients in IC stage can choose observation or intravenous platinum chemotherapy. Patients in II-IV stage are considered to receive systemic adjuvant chemotherapy after surgery. For patients with high ER/PR expression, hormone therapy can be used.
For G2/3 patients, the treatment recommendations are the same as HGSOC, and platinum and paclitaxel chemotherapy after surgery are the first line treatment. PARP inhibitor maintenance treatment after first-line chemotherapy should be considered for platinum sensitive patients in Phase II-IV.
Prognostic factors
The main factors affecting the prognosis are menopausal status, FIGO stage, histological grading, lymph node resection, ascites cytology and hormone receptor expression.
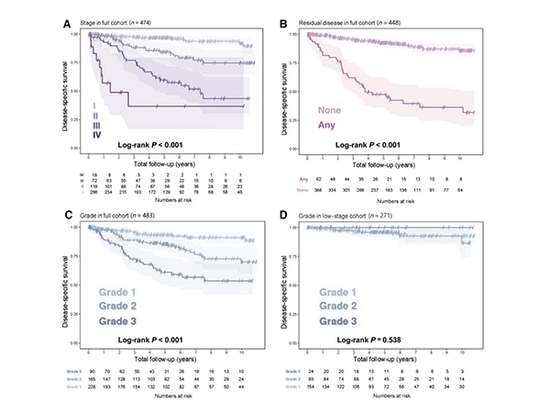
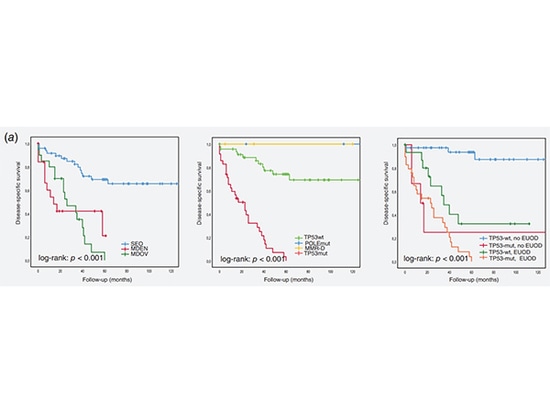
OS, DSS and PFS have significant differences between patients with different FIGO stages and with or without tumor residues (only DSS is shown in the figure above).
The outcome of patients with early stage and no residual tumor was more favorable (P<0.001, Figures A and B).
The prognostic value of histological grading was significant (P<0.001, Figure C), and the prognosis of G3 patients was worse. However, when limited to early (IIA and prior) patients, histological grading no longer had prognostic significance (P=0.538, Figure D).
Some biomarkers also have prognostic value in ENOC, and the high expression of PR and/or ER is a favorable prognostic factor. ARID1A, β-Catenin, TP53, etc. can be used together with routine clinical and histological factors to predict the prognosis of ENOC patients.
Biomarkers
Although the proportion of mismatch repair defect tumors in ovarian cancer is not high, it accounts for 13.8% in endometrioid cancer. NCCN guidelines recommend that all patients with ovarian endometrioid cancer be tested for MSI/MMR.
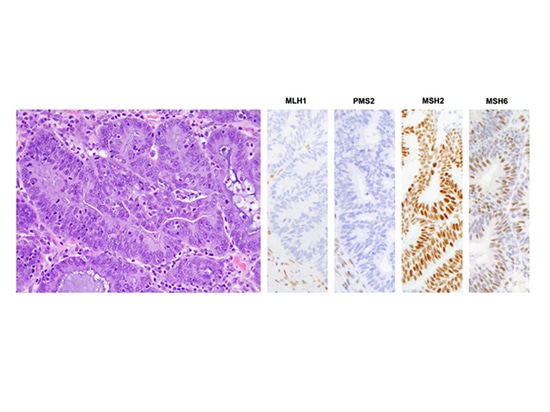
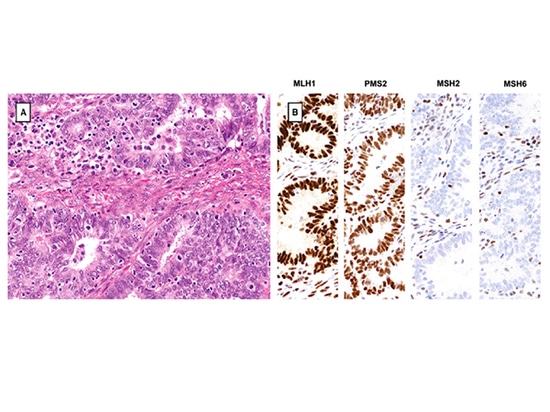
ENOC of dMMR often shows significant TILs and MMR protein deletion (MLH1 and PMS2 deletion in the figure above, MSH2 and MSH6 deletion in the figure below)
Most of the histological subtypes included in the clinical study of ovarian cancer with PARP inhibitor are HGSOC, followed by high-level ENOC; There are also a few mixed cancers, OCCC and undifferentiated cancers. LGSOC and low-grade ENOC were basically not included in clinical research, while mucinous cancer was often included in the exclusion criteria. NCCN guidelines recommend BRCA1/2 gene detection in G2/3 patients with ovarian endometrioid carcinoma at stage II-IV. If BRCA1/2 gene is not mutated, HRD status may provide information about the benefits of PARP inhibitors.
Genotyping in ovarian endometrioid carcinoma
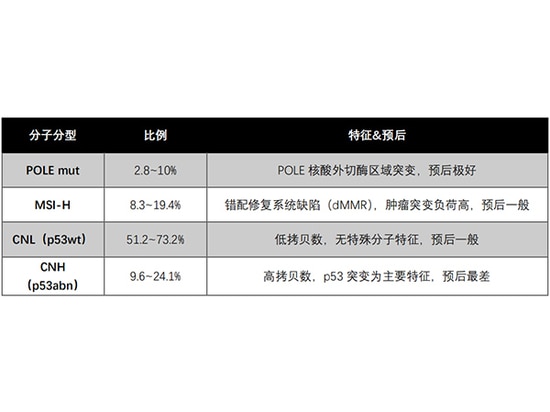
Molecular typing of endometrial cancer has become a routine tool to guide individual treatment and case stratification in clinical trials. ENOC and EEC have many similarities in molecular characteristics and histology, and have similar mutation types, but are different from HGSOC. The following table shows some typing research results in Europe and America.
Genotyping Proportion Characteristics & Prognosis
POLE mut 2.8~10% POLE exonuclease region mutation, excellent prognosis
MSI-H 8.3~19.4% Mismatch repair system defect (dMMR), high tumor mutation load, and general prognosis
CNL(p53wt) 51.2~73.2% Low copy number, no special molecular characteristics, general prognosis
CNH(p53abn) 9.6~24.1% High copy number, p53 mutation as the main feature, with the worst prognosis
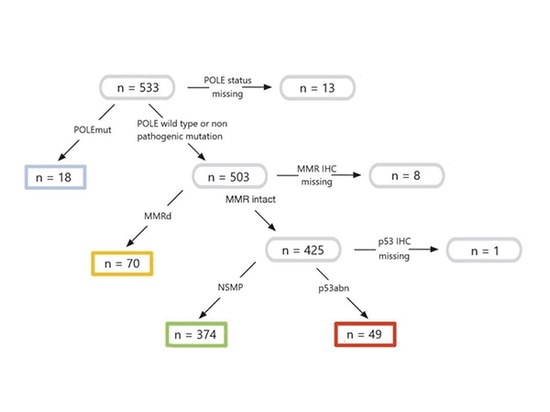
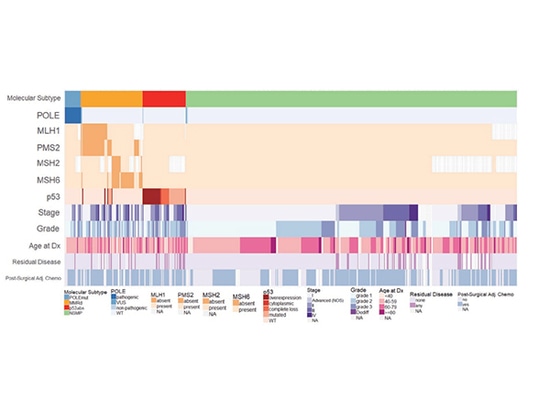
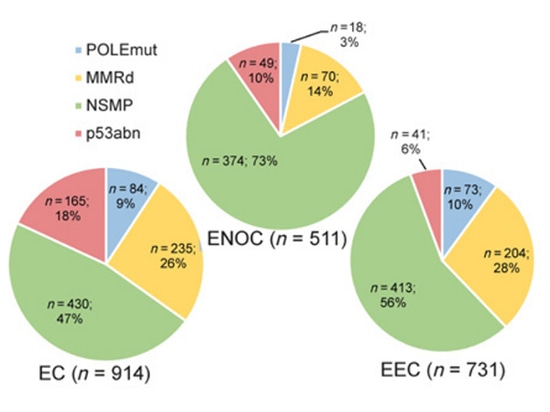
A total of 604 cases of primary ovarian endometrioid cancer were included in four countries and nine centers from Canada and Europe. NGS and Sanger sequencing were used to detect the exonuclease domain of POLE gene in different centers, and IHC was used to detect MMR and p53 protein. A total of 511 cases of ENOC completed molecular typing, of which 3.5% were POLE mut type, 13.7% were MMRd type, 9.6% were p53 abn type, and 73.2% were NSMP type. Compared with EEC, the frequency of POLE mut, MMRd and p53 abn cases in ENOC is lower, while NSMP cases are much more.
Biomarkers and clinicopathological characteristics
Comparison of molecular subtypes of ENOC with EC and EEC
Each molecular subtype showed different prognosis (P<0.001), and the survival period was similar to that observed by EC. During the follow-up period, the median OS of POLE mut type was not reached, 18.1 years for NSMP type, 12.3 years for MMRd type, and 4.7 years for p53 abn type. Based on current research data, it is found that molecular typing and prognostic stratification of endometrial cancer may also be applicable to ovarian endometrioid cancer.
Relationship between ENOC molecular typing and prognosis
Study on genotyping in primary double cancer
The coexistence of endometrial cancer and ovarian cancer is a relatively rare but not rare phenomenon, which may exist in about 10% of patients with ovarian cancer and 5% of patients with endometrial cancer. The patients are generally young (the median age of onset is more than 50 years old), some have high BMI, about 30%~50% of the patients are premenopausal, and some of them have never been pregnant. The common first symptoms were irregular uterine bleeding (30%), postmenopausal bleeding (26.7%), abdominal mass (16.7%) and abdominal pain (26.7%). Endometrioid adenocarcinoma is the most common histological type; The prognosis of patients is generally good. At present, the differentiation between primary double cancer and metastatic cancer is mainly based on the histopathological criteria formulated by Scully.
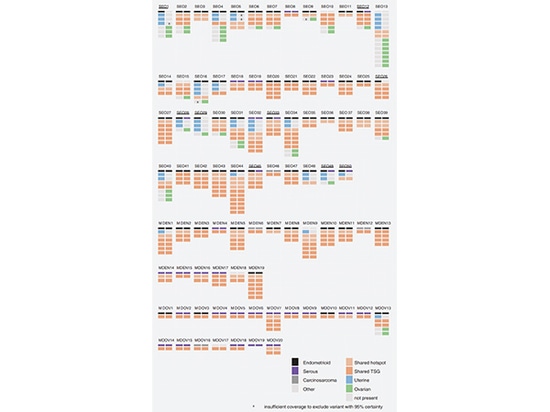
In a retrospective multicenter study, we compared endometrial cancer with ovarian cancer (SEO, n=50), endometrial cancer with synchronous ovarian metastasis (MDEN, n=19), and ovarian cancer with synchronous endometrial metastasis (MDOC, n=20). In 92% (46/50) of SEO, endometrial cancer and ovarian cancer share at least one individual cell mutation, and the clonality index is higher than 0.95, supporting the clonal origin. SEO has a higher frequency of CTNNB1 and PTEN gene mutations, and a lower frequency of TP53 gene mutations. The histology of SEO was consistent in 41 cases, and inconsistent in 9 cases, of which 4 cases had no common mutation, indicating non clonal origin.
Somatic mutation in SEO, MDEN and MDOV
(For each case, endometrial cancer mutations are shown in the left column, ovarian cancer mutations are shown in the right column, and shared mutations are orange)
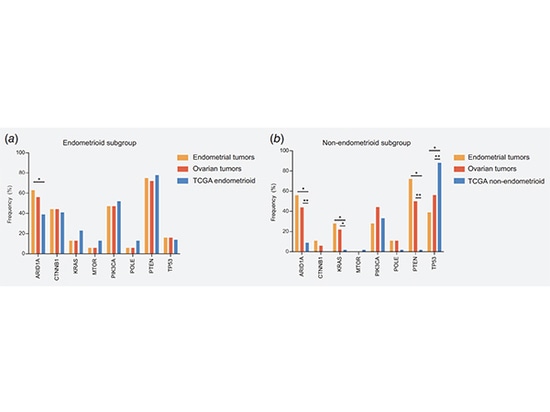
The mutation spectrum of SEO subgroup was compared with that of TCGA endometrial carcinoma: (a) Endometrioid carcinoma in the cohort (n=32) was compared with that in TCGA dataset (n=193); (b) Non endometrioid carcinoma (n=18) in the cohort was compared with serous carcinoma (n=43) in the TCGA dataset. The consistency is high, suggesting the endometrium origin of SEO.
Comparison of mutation spectrum between SEO subgroup and TCGA endometrial carcinoma
The ProMisE classification method was used to identify four subtypes with significant prognostic differences. SEO has a better outcome than MDEN and MDOC (left in the figure below).TP53 mut (in the figure below) and extrauterine ovarian disease (in the right figure below) are independent poor prognostic factors.
KM curve shows DSS of the case
Summary
ENOC is one of the important subtypes of ovarian cancer. Similar to endometrial cancer, the prognosis of ENOC is heterogeneous. There have been some reports on the research of molecular typing in ENOC, and the application of molecular typing in ovarian cancer has also been mentioned in WHO Cancer Classification 5th Edition: Female Reproductive System Tumor. The diagnosis of SEO still has challenges. NGS technology and molecular typing will help to further clarify the diagnosis.
The molecular typing of endometrial cancer of SpaceGen Biological adopts the method of high-throughput sequencing, and comprehensively detects the typing markers and auxiliary typing factors recommended by the guidelines, which has implications for the prognosis, auxiliary treatment, immunotherapy, hormone therapy and genetic risk of endometrial cancer patients. SpaceGen is committed to providing the most innovative products and services for individualized precise medical detection of tumors and continues to update existing products.
Reference
[1] IARC 2020 World's Latest Cancer Burden Data
[2] Front Oncol. 2021 Jun 3;11:668151.
[3] WHO Cancer Classification 5th Edition: Female Reproductive System Tumors
[4] NCCN Guidelines for Diagnosis and Treatment of Ovarian Cancer 2023 v1
[5] Clin Cancer Res. 2020 Oct 15;26(20):5400-5410.
[6] Am J Surg Pathol. 2012 Feb;36(2):163-72.
[7] Histopathology. 2016 Aug;69(2):288-97.
[8] Cureus. 2020 Jul 13;12(7):e9163.
[9] Arch Gynecol Obstet. 2012 Mar;285(3):817-21.
[10] Int J Cancer. 2020 Jul 15;147(2):478-489.
[11] Gynecol Oncol. 2004 Aug;94(2):456-62.