#Industry News
Is an undeniable thyroid nodule truly terrifying?
Is an undeniable thyroid nodule truly terrifying?
In recent years, with the improvement of living standards and health risk awareness, physical examinations have become an essential means of monitoring one's health status. As the regulator of metabolic activities and often referred to as the "engine of the human body," the endocrine organ - thyroid, which is closely related to bodily functions, is included in most of the medical examination procedures. Thyroid nodules are commonly found in the female population, with a detection rate of 3% to 7% through palpation, and a detection rate as high as 20% to 76% through high-resolution ultrasound. In a nationwide epidemiological survey called the Thyroid Disease, Iodine Nutrition, and Diabetes Epidemiology (TIDE) project, which included 78,470 adults aged 18 and above from 31 provinces and municipalities in China, the prevalence of thyroid nodules was 20.43% (nodules with a diameter > 0.5cm). So, what exactly are thyroid nodules? What are the available methods for detecting thyroid nodules? How are thyroid nodules treated?
1. What is a thyroid nodule?
Concept: A thyroid nodule refers to a discrete abnormality caused by the focal growth of thyroid cells within the thyroid gland. It can be caused by various factors, and clinically, there are multiple thyroid disorders such as thyroid inflammation, autoimmune conditions, and neoplasms that can manifest as nodules.
2. Nature:
- Hyperplasia (e.g., simple or nodular goiter)
- Inflammation (e.g., thyroiditis such as subacute thyroiditis or chronic lymphocytic thyroiditis)
- Malignant tumors (e.g., metastatic carcinoma, parathyroid tumors, etc.)
3. Clinical presentation: Most thyroid nodules do not exhibit clinical symptoms. However, some patients may experience symptoms due to the compression of surrounding thyroid tissues, leading to hoarseness, pressure sensation, difficulty breathing, and swallowing difficulties. Malignant nodules tend to grow rapidly, cause persistent hoarseness or difficulty in speaking without vocal cord issues, have irregular shapes, adhere to and fixate on surrounding tissues, and may lead to pathological enlargement of neck lymph nodes.
symptoms
difficulty swallowing
swollen neck
hoarseness
difficulty breathing
lump in the neck
What are the common detection methods for thyroid nodules?
1. Thyroid hormone (thyroid function three items FT3, FT4, TSH) detection: to determine whether the thyroid function is abnormal, and those with elevated TSH need to measure thyroid autoantibodies.
2. Detection of thyroid autoantibodies (TGAb, TRAb, TPOAb)
3. Detection of tumor markers (globulin (Tg), calcitonin, carcinoembryonic antigen (CEA))
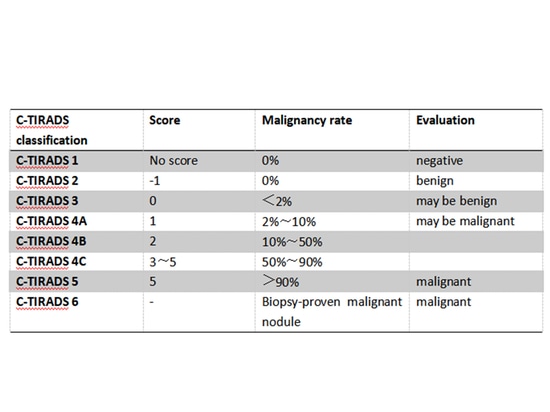
4. Imaging (ultrasound) detection: the preferred examination method for all known or suspected thyroid nodules, which helps to distinguish benign and malignant thyroid nodules, and can use the Chinese version of Thyroid Imaging Reporting and Data System (C-TIRADS) predict its risk of malignancy. Research data show that: 8% to 16% of thyroid nodules are malignant, that is, thyroid cancer.
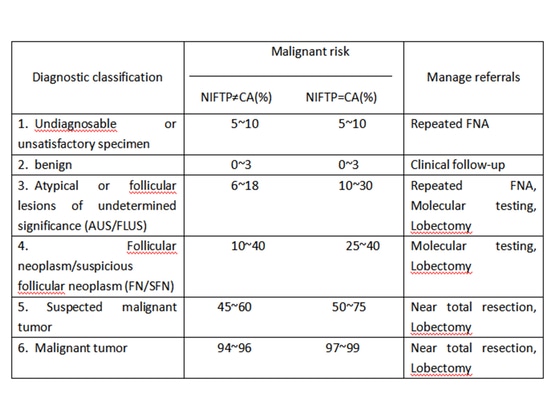
5. Ultrasound-Guided Fine-Needle Aspiration (US-FNA): This involves using a fine needle to aspirate cells from a thyroid nodule under ultrasound guidance for pathological examination. It is a diagnostic method used to determine whether a thyroid nodule is benign or malignant.
6. Genetic Testing: In cases where the nature of a thyroid nodule (Bethesda III/IV) cannot be definitively determined even after US-FNA, molecular marker testing can be performed on the biopsy specimen. Testing for genetic mutations such as BRAF, RAS mutations, RET/PTC rearrangements, etc., can help increase the accuracy of diagnosis and aid in developing personalized treatment plans.
III、How are thyroid nodules treated?
The majority of benign thyroid nodules only require regular follow-up, and benign nodules that are asymptomatic and not rapidly growing generally do not require specific treatment. In a few cases, options for treatment include surgical intervention, medical management (such as TSH suppression therapy), radioactive iodine (131I) therapy, and ablative therapy. For nodules classified as Bethesda III/IV with BRAF gene mutations or combined with other gene mutations, suspicious characteristics on ultrasound, larger nodules (diameter > 4 cm), a family history of thyroid cancer, or a history of radiation exposure, due to the higher risk of malignancy, diagnostic surgical excision is recommended. The following are treatment approaches for benign nodules:
1. Surgical Treatment
There is no absolute size criterion for benign thyroid nodules that require surgical treatment. Typically, for Bethesda II nodules, a diameter greater than 3-4 cm is associated with an increased risk of malignancy. In some cases, patients with asymptomatic benign nodules might opt for surgery if the nodule's size significantly impacts their appearance or causes considerable psychological distress affecting their daily life and work. This can also be considered a relative indication for surgery.
2. Medical Management (TSH Suppression Therapy)
There are generally no specific medical treatment protocols for benign thyroid nodules. It is important to avoid risk factors that might promote nodule growth, such as hypothyroidism, iodine deficiency, smoking, ionizing radiation exposure to the head and neck, obesity, and metabolic syndrome. TSH suppression therapy is not recommended for patients with benign thyroid nodules and normal thyroid function. Prolonged use of this therapy can lead to discomforting symptoms like cardiac arrhythmias and exacerbate osteoporosis in postmenopausal women.
3. 131I treatment
131I is mainly used to treat benign thyroid nodules with autonomous uptake function and hyperthyroidism. If hypothyroidism occurs, LT4 replacement therapy should be given in time.
4. Ablative Therapy
Ablative therapy is an option for patients with benign thyroid nodules that are progressively enlarging, causing compression symptoms, affecting appearance, causing significant psychological distress impacting daily life, and who are unwilling to undergo surgery. However, it's important to note that before undergoing ablative therapy, an ultrasound-guided fine-needle aspiration (US-FNA) must be performed to confirm the pathological diagnosis as benign. Even after ablative therapy, long-term follow-up is necessary.
Monitoring and Screening for High-Risk Individuals
Individuals with the following medical histories are considered to be at high risk for thyroid cancer and should undergo early screening:
1. History of childhood head and neck radiation exposure or exposure to radioactive dust.
2. History of systemic radiation therapy.
3. First-degree relatives with a history of thyroid cancer, as well as a family history of thyroid cancer-related hereditary syndromes or personal history of such syndromes.
References
[1] JAMA, 2018, 319(9): 914-924.
[2]Thyroid,2020,30(4):568-579.
[3] Guidelines for the diagnosis and treatment of thyroid nodules and differentiated thyroid cancer (second edition)
[4] Guidelines for Diagnosis and Treatment of Thyroid Cancer (2022 Edition)