#Industry News
The Matters Between Thyroid Cancer and the RET Gene
The Matters Between Thyroid Cancer and the RET Gene
In the previous issue, we discussed the relationship between the BRAF gene and thyroid cancer (see "The Matters Between Thyroid Cancer and the BRAF Gene"). In this issue, we will focus on the RET gene and unravel the mysteries surrounding the relationship between the RET gene and thyroid cancer.
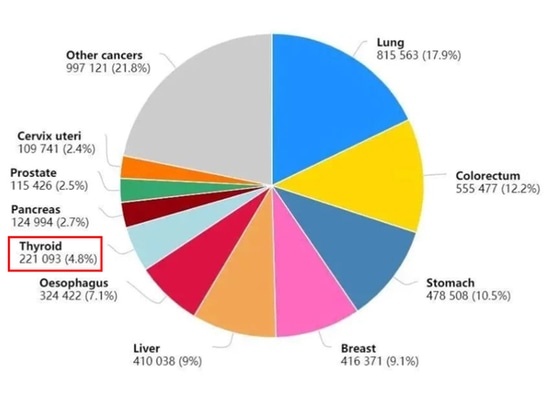
Figure 1: Top Ten New Cancer Cases in China in 2020
In recent years, the incidence of thyroid cancer has shown a sustained and rapid increase globally, including in China. The worldwide annual number of new cases is close to 600,000, with Chinese patients accounting for over one-third of this total (Figure 1). The ratio of female to male patients is approximately 3:1 [1].
The RET gene, discovered in 1985, is an oncogene located on the long arm of chromosome 10 (10q11.2), spanning approximately 60 kb and consisting of 21 exons. The RET gene encodes a receptor tyrosine kinase protein that regulates cell proliferation, growth, differentiation, migration, and apoptosis. It also plays a crucial role in organ development and the nervous system development process, as well as being associated with male sperm production [2].
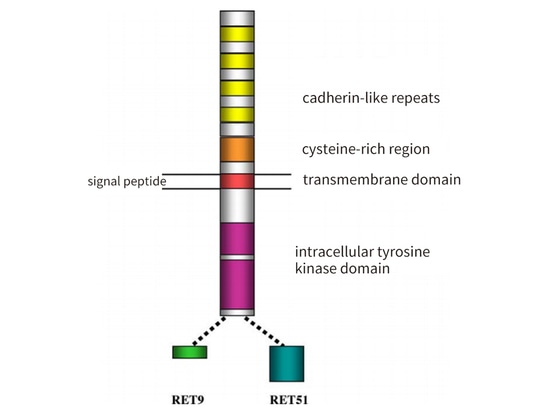
The RET protein consists of three domains: an extracellular domain with four calcium-binding protein-like repeat sequences and a region rich in cysteine; a transmembrane domain; and an intracellular tyrosine kinase domain. The RET protein has three subtypes: RET 51 (long 51-amino acid), RET 43 (medium 43-amino acid), and RET 9 (short 9-amino acid). They exhibit differences in temporal and spatial regulation, cellular localization and transport, as well as biological functions. Among them, RET 51 and RET 9 are the main subtypes, both highly conserved, but RET 51 is more effective than RET 9 in promoting cell proliferation, migration, and anchoring [3] (Figure 2).
Figure 2: Schematic Representation of the Structure of the RET Protein
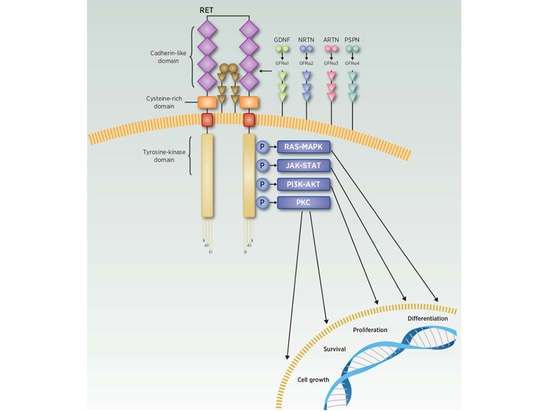
How does the RET gene participate in regulating the cell growth cycle? And how does it lead to the occurrence of tumors? The RET protein is involved in cellular signaling pathways such as RAS-MAPK, PI3K-AKT, JAK-STAT, and PKC, participating in processes such as cell growth, proliferation, differentiation, and apoptosis throughout the cell cycle. However, only the activated RET protein can activate downstream signaling pathways and play a regulatory role. Current research indicates that the activation of the RET protein requires the involvement of both the glial cell line-derived neurotrophic factor (GDNF) family ligands (GFLs) and the GDNF family receptor-α (GFRα). There are various types of GFLs, including not only GDNF but also neurturin (NRTN), artemin (ARTN), and persephin (PSPN). When the ligands GDNF, NRTN, ARTN, and PSPN bind to the receptors GFRα1, GFRα2, GFRα3, and GFRα4, respectively, the GFLs-GFRα complex binds to RET, triggering its homodimerization, phosphorylation of tyrosine residues, and subsequent intracellular signal transduction, thereby participating in the regulation of the cell growth cycle [4-5] (Figure 3).
Figure 3 RET signal transduction pathway
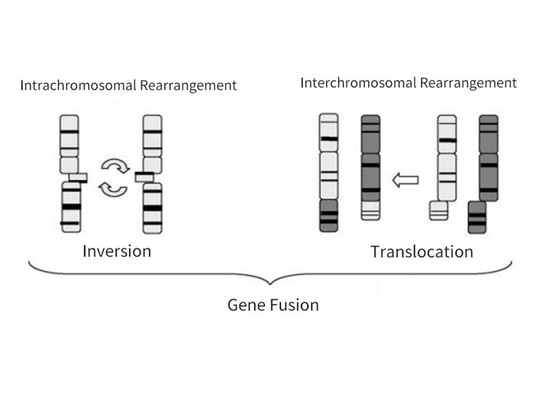
1.Papillary thyroid cancer (PTC) with RET gene mutations
Thyroid cancer is the most common malignant endocrine tumor, originating from the thyroid follicular epithelium or parafollicular epithelial cells (Figure 4). According to the origin and differentiation, thyroid cancer can be divided into Differentiated Thyroid Cancer (DTC), Medullary Thyroid Cancer (MTC), Poorly Differentiated Thyroid Cancer (PDTC), and Anaplastic Thyroid Cancer (ATC). Among them, DTC is further divided into Papillary Thyroid Cancer (PTC) and Follicular Thyroid Cancer (FTC). Among all histological types, PTC is the most common, accounting for about 90% of all thyroid cancers, while MTC is relatively rare, accounting for about 3%. Studies have shown that RET gene mutations most commonly occur in PTC and MTC, with PTC primarily experiencing RET rearrangement and MTC mainly having RET mutations. Compared to the most common BRAF mutations in PTC, RET rearrangement is not very common in PTC, accounting for about 10% to 20%, and RET rearrangement and BRAF mutations are mutually exclusive. RET gene breakpoints often occur in intron 11, occasionally in introns 7 and 10, leading to inversion or translocation of the kinase domain's 3' end and the 5' end of other partner genes. This activation of RET kinase produces chimeric oncoproteins, ultimately leading to the development of tumors [6-8] (Figure 5).
Figure 5: RET Rearrangement
So far, there have been more than 35 genes that have formed fusion genes with RET, among which CCDC6-RET and NCOA4-RET are the most common in papillary thyroid carcinoma (PTC), named RET/PTC1 and RET/PTC3 respectively, accounting for 60% and 30% of PTC RET rearrangement types (Figure 6). Ionizing radiation is a common factor leading to RET rearrangement. According to reports, the incidence of RET rearrangement in PTC patients who were exposed to Chernobyl radioactive fallout or affected by the atomic bombs in Japan is 50% to 80%. Additionally, it is more common in children than in adults. Young thyroid cancer patients with RET rearrangement often exhibit early extracapsular invasion, lymph node metastasis, and distant metastasis, resulting in a higher stage. Retrospective studies have shown that the malignant diagnosis rate of Bethesda category III nodules with RET/PTC rearrangement is 60%, with no false positives, indicating that RET/PTC rearrangement is a highly specific marker for PTC diagnosis. The consensus among experts in China recommends early and active surgical treatment for PTC with RET rearrangement [6-8].
Figure 6 Main types of RET rearrangements (thyroid cancer)
2. RET Gene Variants in Medullary Thyroid Carcinoma (MTC)
MTC is a malignant tumor caused by the secretion of calcitonin (Ctn) from parafollicular C cells. Based on the genetic characteristics of the disease, MTC is classified into hereditary (20%~25%) and sporadic (75%~80%) types. Almost all cases of hereditary MTC (HMTC) are associated with germline mutations in the RET gene, inherited through autosomal dominant inheritance. Fifty percent of sporadic MTC cases have somatic mutations in the RET gene. HMTC is part of Multiple Endocrine Neoplasia Type 2 (MEN2) and can be further categorized into three subtypes based on clinical features: MEN2A, MEN2B, and Familial Medullary Thyroid Carcinoma (FMTC). MEN2A is the most common subtype, accounting for 60%~90% of MEN2 families; MEN2B represents 5%, with a higher degree of malignancy; FMTC is the most indolent subtype of MEN2, manifesting later in life [7, 9].
1. RET Gene Mutations and MEN2A
Ninety-five percent of MEN2A patients with RET gene mutations exhibit hotspots in six cysteine residues rich in extracellular regions of the RET protein. These residues are mainly located in codons 609, 611, 618, and 620 of exon 10, as well as codons 630 and 634 of exon 11. Cysteine residues at these sites are frequently replaced by other amino acids, reducing intramolecular disulfide bond formation. This promotes the formation of RET homodimers through intermolecular disulfide bonds, leading to sustained activation of RET in the absence of ligands [7, 9, 10] (Figure 7).
2. RET Gene Mutations and FMTC
In FMTC patients, RET mutations are found not only in extracellular cysteine residues but also in other non-cysteine residues both extracellularly and intracellularly. Examples include Gly533Cys (G533C) in exon 8 of the extracellular domain, Glu768Asp (E768D), Leu790Phe (L790F), Tyr791Phe (Y791F), Val804Met/Leu (V804M/L), and Ser891Ala (S891A) in exons 13-15 of the kinase domain [7, 9, 10] (Figure 7).
3. RET Gene Mutations and MEN2B
MEN2B patients have mutations related to the RET gene kinase domain. Ninety-five percent of MEN2B patients carry the M918T mutation in exon 16 of the RET gene, while less than 5% carry the A883F mutation in exon 15. These mutations can alter protein conformation, increase ATP binding affinity, and reduce self-inhibition [7, 9, 10] (Figure 7).
Figure 7 MEN2 family RET gene mutation types
4.RET Gene Mutations and Sporadic Medullary Thyroid Carcinoma (MTC)
Sporadic MTC mostly involves somatic mutations in the RET gene. The most common site is M918T (approximately 80%), followed by the second most common mutation site, C634 mutation (around 15%). Other rare somatic mutations involve sites such as A883, C609, C630, among others. Studies indicate that the RET gene M918T somatic mutation is associated with the invasiveness of MTC. Therefore, guidelines recommend testing for somatic RET mutations in patients with advanced MTC or those planning selective RET inhibitor therapy. Despite being a sporadic disease, research shows that 1% to 7% of sporadic MTC patients actually have hereditary diseases. Therefore, the guidelines suggest that sporadic MTC patients undergo genetic counseling and testing for RET mutations. In sporadic MTC, RET mutations are mutually exclusive with HRAS and KRAS mutations [7, 9, 10].
5.Stratification of Risk for RET Gene Mutation Sites
Currently, over 100 types of point mutations, copy number variations, insertions, or deletions in the RET gene have been found to be associated with hereditary MTC. The malignancy of tumors caused by different mutation sites varies, and they can be classified into the highest-risk group, high-risk group, and moderate-risk group (Figure 8). Different preventive and treatment strategies will be employed based on the varying degrees of risk [7, 9, 10].
Figure 8 RET gene mutation sites and the malignant risk of hereditary medullary thyroid cancer
In summary, RET gene variation is closely associated with thyroid cancer, especially in papillary thyroid cancer (PTC) and medullary thyroid cancer (MTC). RET/PTC rearrangement can also be used as a marker for the diagnosis of benign and malignant thyroid nodules. It can also assist in the diagnosis of hereditary thyroid risk and provide timely prevention.
SpaceGen's thyroid cancer gene mutation detection is conducive to scientifically and accurately assessing an individual's risk of thyroid cancer and formulating a personalized management plan.
References
[1]IARC 2020 latest global cancer burden data.
[2]Cytokine & growth factor reviews,2005,16(4-5): 441-467.
[3]Cytogenet Cell Genet 2001,95:169-76.
[4]Nature reviews Clinical oncology,2018,15(3):151-167.
[5]JMA J, 2020, 3(3): 175-181.
[6] Thyroid Cancer Diagnosis and Treatment Guidelines (2022 Edition)
[7]Expert Consensus on RET Gene Testing and Clinical Application of Thyroid Cancer (2021 Edition)
[8] Guangdong Expert Consensus on Gene Testing and Clinical Application of Thyroid Cancer (2020 Edition)
[9] Chinese Expert Consensus on Diagnosis and Treatment of Medullary Thyroid Cancer (2020 Edition)
[10] CSCO Guidelines for Diagnosis and Treatment of Medullary Thyroid Cancer (2022 Edition)