#Industry News
Do you know the silent killer pulmonary embolism?
Pulmonary Artery I
To sum it up in one sentence: Pulmonary embolism has the characteristics of sudden onset, easy misdiagnosis, high death rate and limited treatment methods. It is a disease that makes doctors blush and hate it very much. It can also be said to be a typical "silent killer" .
Pulmonary embolism (PE) is a disease of pulmonary circulation disorder caused by "emboli" blocking the pulmonary artery and its branches.
Although there are many "emboli" that can cause pulmonary embolism, including thromboembolism, fat embolism, amniotic fluid embolism, air embolism, tumor embolism , etc., the vast majority of clinical cases are pulmonary thromboembolism (PTE), that is, Pulmonary embolism caused by thrombus from the venous system or right ventricle, especially thrombus from the lower limbs or deep pelvic veins, is the main "culprit" of pulmonary thromboembolism.
So what are the "terrible things" about pulmonary embolism? Boston Scientific will give you a brief introduction to science.
one. Pulmonary embolism often occurs suddenly and has a high rate of death and disability.
Pulmonary thromboembolism is a very dangerous disease, especially acute pulmonary embolism caused by deep vein thrombosis, which often occurs suddenly, resulting in a short time for clinical treatment. Once the pulmonary artery lumen is blocked, it will directly cause pulmonary circulation and respiratory dysfunction. If it is an acute severe pulmonary embolism, it may cause death within 30 to 120 minutes.
1. Once the lumen of the pulmonary artery is severely blocked, it may be difficult for the blood in the heart to pump to the pulmonary artery, and the blood pressure of the pulmonary artery increases, which in turn causes the right ventricle afterload to be too large, which can lead to right ventricle failure in a short time , and then lead to sudden death of the patient.
At the same time, pulmonary embolism can also lead to reduced blood flow in the lungs. When there is not enough blood flowing into the alveoli to complete gas exchange, the oxygen content in the blood will drop sharply, resulting in varying degrees of respiratory dysfunction. Exhausted.
According to the current epidemiological model, in the six EU countries with a total population of 454.4 million in 2004, there were more than 317,000 deaths from acute pulmonary embolism, but among them, sudden fatal acute pulmonary embolism accounted for 34%, and more than 59% of patients were not diagnosed before death [1] . In the ten years from 2007 to 2016, the hospitalization rate due to pulmonary embolism in my country increased from 1.1 per 100,000 people to 6.3 per 100,000 people. Although the mortality rate has been declining year by year with the improvement of medical technology and diagnosis rate, the in-hospital mortality rate due to this disease in 2016 was still as high as 3.9% .
2. pulmonary embolism is difficult to diagnose and is easily misdiagnosed and missed.
Although acute pulmonary embolism is a common cardiovascular disease, due to the lack of specific symptoms and signs, as well as the difficulty and high cost of examination, it is easy to be misdiagnosed, missed and diagnosed in a timely manner.
Patients with acute pulmonary embolism may have symptoms such as fatigue, dyspnea, chest pain, dizziness, fever, and hemoptysis, so most patients with such symptoms will be suspected of acute pulmonary embolism. However, there are a large number of clinical patients who have few or no obvious symptoms, and even the first symptom is sudden death. Therefore, pulmonary embolism is often accidentally discovered during the diagnosis of other diseases or autopsy.
Due to the lack of specific signs, acute pulmonary embolism is difficult to diagnose directly through routine examinations such as chest X-ray and electrocardiogram. However, examinations such as multi-slice spiral CT and pulmonary angiography that can clearly diagnose pulmonary embolism require the patient to lie flat and fully cooperate. The cost is relatively high, and many primary hospitals are not equipped with such examination equipment.
3. Treatment options are limited, making it difficult for severely ill patients to receive effective treatment.
For the treatment of pulmonary thromboembolism, anticoagulation, thrombolysis, catheter intervention, surgical thrombectomy, drug anticoagulation and other treatments are currently commonly used. Severe cases may require surgical thrombectomy or extracorporeal membrane oxygenation (ECMO).
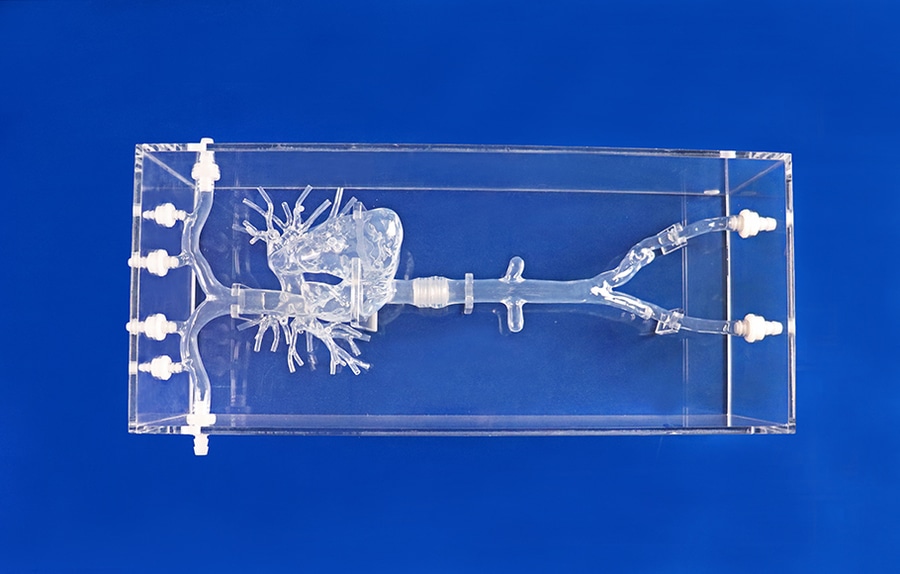
The main treatment methods of catheter intervention include physical thrombus fragmentation, suction catheter rotation and aspiration, and catheter thrombolysis. Among them, catheter thrombolysis (CDT) treatment uses a catheter to inject thrombolytic drugs into the target thrombus site to achieve the purpose of drug thrombolysis. However, due to the slow onset of thrombolytic drugs and the long time it takes to take effect (up to 7 days), it is often difficult for patients with severe embolism to receive timely and effective treatment . and bleeding or clot shedding caused by anticoagulant drugs .
These various reasons have caused pulmonary embolism to become a problem that many doctors are afraid of.
Fortunately, technology has been improving, and an "advanced version" of ultrasonic catheter thrombolysis technology is already being used abroad.
Specifically, ultrasonic catheter thrombolysis combines traditional catheter thrombolysis with ultrasonic oscillation technology, that is, while infusing thrombolytic drugs, high-frequency, low-energy ultrasound is used to oscillate the tight thrombus tissue in the target area to a loose state. This allows the drug to better penetrate into the thrombus and accelerate the effect of dissolving the thrombus. This treatment requires only a very small amount of thrombolytic drugs to achieve rapid thrombolysis, and further reduces the risk of major bleeding by reducing the amount of drugs used.
For patients with contraindications to thrombolytic treatment, failure of thrombolytic treatment, or severe patients who have suffered cardiogenic shock before thrombolytic treatment, the pulmonary artery must be cut to directly remove the thrombus , and "evisceration" is inevitable. .
In general, pulmonary embolism has a high incidence rate and is difficult to diagnose and treat. It is no wonder that it has become the third leading cause of cardiovascular death after coronary heart disease and stroke.





