#Industry News
Atrial Septal Defect
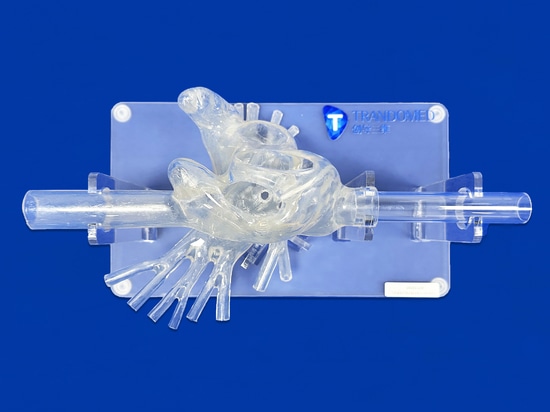
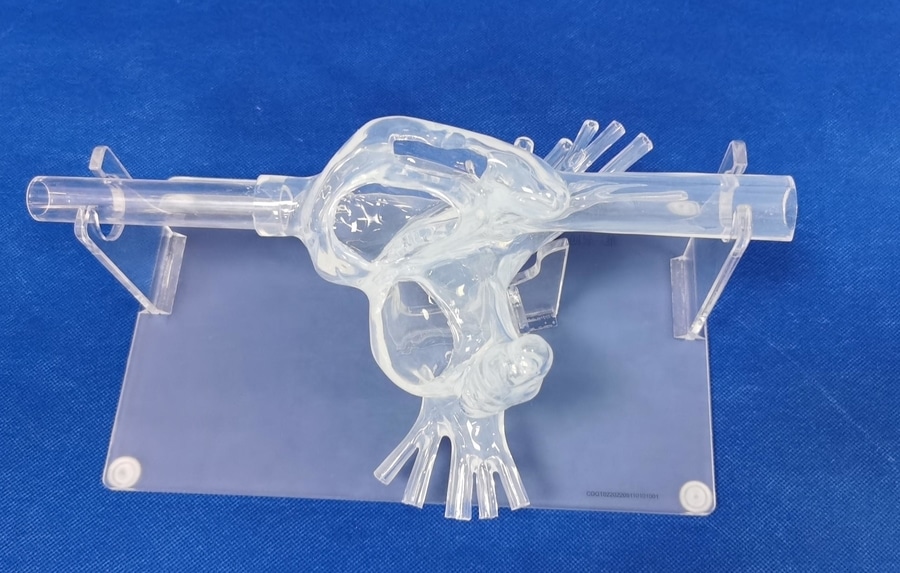
Model:Heart Model with ASD
Atrial septal defect (ASD) is one of the common congenital heart diseases in children, caused by incomplete development of the septum between the left and right atria, leading to an abnormal pathway between the two chambers.
Etiology and Pathogenesis
1.Etiology: Related to intrauterine environmental factors during fetal development, maternal conditions, and genetic factors.
2.Classification: Atrial septal defects can be classified into primary septal defects and secondary septal defects.
• Primary Septal Defects: Located below the anterior inferior vena cava, with the lower edge of the defect close to the tricuspid valve annulus, often associated with atrioventricular septal defects.
• Secondary Septal Defects: More common, located above the posterior superior vena cava. The vast majority are single defects, with a few being multiple defects or fenestrated defects. Based on the anatomical location of the defect, they are further classified as central type (oval foramen type), superior vena cava type (vena cava type), inferior vena cava type, and mixed type. Secondary septal defects are often associated with other cardiac malformations, such as pulmonary valve stenosis and tricuspid valve stenosis.
Pathophysiology
In a normal state, the pressure in the left atrium is higher than that in the right atrium. With an atrial septal defect, blood from the left atrium flows through the defect to the right atrium, and the amount of shunting depends on the pressure difference between the two atria, the size of the defect, and the resistance to filling of the left and right ventricles. In newborns, the pressures in the two atria are similar, resulting in minimal shunting; as they grow older, the pressure difference between the atria increases, leading to increased right-to-left blood flow, sometimes reaching 2 to 4 times the systemic blood flow.
Increased right heart volume load leads to enlargement of the right atrium, right ventricle, and pulmonary artery dilation. The increased blood volume in the pulmonary circulation raises pulmonary artery pressure, triggering reactive spasm of the pulmonary arterioles. Long-term spasm causes intimal proliferation, medial thickening, fibrosis, luminal narrowing, increased pulmonary vascular resistance, and eventually leads to obstructive pulmonary arterial hypertension. When right atrial pressure exceeds left atrial pressure, right-to-left shunting occurs, resulting in cyanosis, Eisenmenger syndrome, and ultimately death due to right heart failure.
Clinical Manifestations
1.Symptoms: Patients with small shunts in secondary atrial septal defects may have no obvious symptoms in childhood and are often detected during routine physical examinations. Typically, symptoms such as exertional dyspnea, fatigue, palpitations, respiratory infections, and right heart failure appear in young adults. In primary atrial septal defects with severe tricuspid regurgitation, early symptoms may include heart failure and pulmonary arterial hypertension. Severe pulmonary arterial hypertension can cause right-to-left shunting and cyanosis.
2.Signs:
• Inspection: Enlargement of the heart is evident in primary atrial septal defects, with prominence in the precordial area. Cyanosis and clubbing of the fingers and toes may be present in secondary atrial septal defects.
• Palpation: A lifting impulse may be felt in the precordial area, and in some cases, a thrill may be palpable.
• Auscultation: A II-III grade blowing systolic murmur may be heard in the pulmonary valve area, accompanied by accentuated second heart sound and fixed splitting. In cases of significant shunting, a soft diastolic murmur may be heard at the apex. In patients with pulmonary arterial hypertension, the systolic murmur in the pulmonary valve area diminishes, the second heart sound intensifies, and splitting is more pronounced.
Introducing the Heart Model with ASD, a comprehensive educational tool designed to enhance understanding and practice in the field of cardiology. This intricately detailed model features components essential for studying atrial septal defects (ASD), including the left and right atria, pulmonary veins, superior vena cava (SVC), inferior vena cava (IVC), left atrial appendage (LLA), right atrial appendage (RAA), and the foramen ovale. Mounted on a transparent acrylic plate, this model offers a clear view of the internal structures, facilitating interactive learning experiences.
Noteworthy for its versatility, this heart model is not only informative but also functional in medical simulations. With applications ranging from simulating foramen ovale puncture to practicing pulmonary vein ablation and left atrial appendage occlusion procedures, it serves as a valuable tool for medical training and procedure rehearsal. Moreover, the customization options available for this model further enhance its utility, enabling tailored adjustments such as resizing the foramen ovale, incorporating additional common lesions like ventricular septal defects (VSD) and patent ductus arteriosus (PDA), and even creating personalized models based on provided data files in various formats like CT scans, CAD designs, and STL files.