#Industry News
Surgical Embolectomy for Acute Pulmonary Thromboembolism
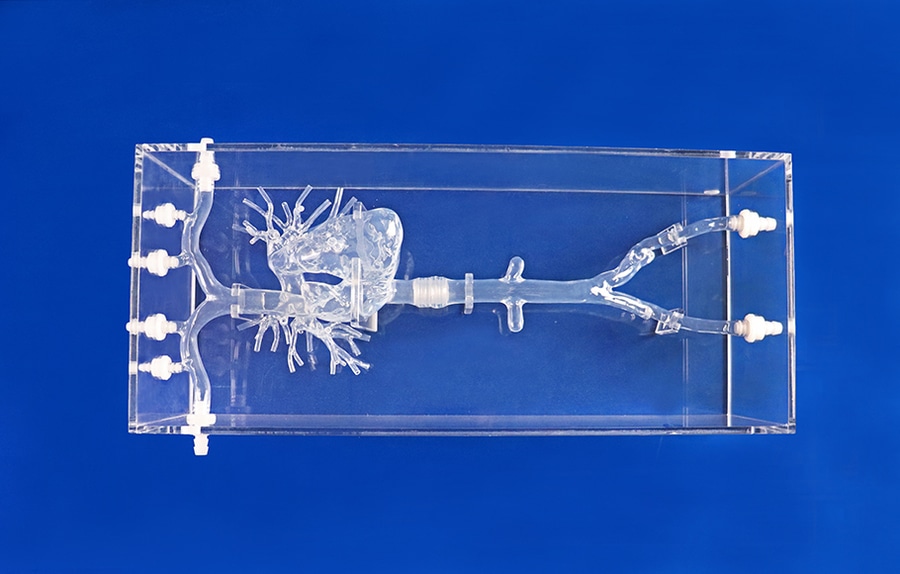
Pulmonary Artery I
Acute pulmonary thromboembolism (PE) was one of the major cardiopulmonary menaces to hospitalized patients before the advent of anticoagulant therapy using heparin. In 1906, Friedrich Trendelenburg in Leipzig reported the ligation of the inferior vena cava to prevent the progression and embolization of septic thrombi in puerperal sepsis. He also attempted an “off-pump” pulmonary embolectomy via a left small thoracotomy in patients with a femoral neck fracture in 1908. This procedure was based on experimental study; in fact, the patient died of bleeding during the operation. No patient survived this procedure until the first successful report from Martin Kirschner, Trendelenburg’s former trainee, in 1924. It was a very difficult procedure with extremely high mortality; thus, it was performed only for critically ill patients, resulting in highly unreliable and uncertain outcomes. The idea of extracorporeal circulation inspired John Gibbon to develop cardiopulmonary bypass during his care of a patient with massive PE in 1931. The initial idea was to apply extracorporeal circulation to treat massive PE, and he began research on extracorporeal circulation. In 1936, clinical application of heparin as pharmacological prophylaxis and treatment of venous thromboembolism was introduced, 30 years after the discovery of heparin in 1916. With the development of the heart-lung machine and the use of heparin as an anticoagulant, Denton Cooley and his colleagues performed pulmonary embolectomy using cardiopulmonary bypass in 1961. They also reported the use of “portable” cardiopulmonary bypass as a bridge to surgical pulmonary embolectomy. However, after the advent of thrombolytic therapy in the 1970s, surgical pulmonary embolectomy was criticized as an obsolete therapeutic modality because patients who needed pulmonary embolectomy were too ill to transport to a specialized heart center. Thrombolytic therapy is effective for resolving clots in the pulmonary artery; however, most studies have not shown that thrombolytic therapy has a survival advantage because of the risk of critical hemorrhage.
The pulmonary circulation has a huge capillary bed because the entire systemic venous return goes into the pulmonary circulation. The pulmonary capillary bed covers nearly the entire alveoli area, with a total surface area of 100–140 m2. Because the pulmonary vasculature has a wide endothelial area, the lung has strong endogenous fibrinolytic properties.
Most pulmonary thromboemboli are generated in the venous bed of the lower extremities as deep vein thromboses. The deep venous system consists of multiple tracts embedded between muscular compartments. The venous walls are thin and highly stretchable, working as capacitance vessels and a reservoir of blood. The deep veins of the extremities have bileaflet valves to prevent regurgitation of venous blood to the feet. There are many venous sinuses in the calf muscles, especially in the soleus muscle, draining into the posterior tibial and peroneal veins. The soleal sinuses are large, short, thin-walled, and valveless. They are embedded in the soleus muscle, working as a “peripheral heart” during ambulation to eject pooled blood and resisting 80 mmHg of pressure from gravity below the heart. However, the soleal sinuses may become cradles of deep vein thrombi if patients are on long-term bed rest or immobilization by a cast combined with other thrombogenic factors such as thrombophilia or intimal injury. Thrombi in soleal venous sinuses extend to the proximal veins, forming a long, sausage-shaped thrombus.
From the anatomical perspective, the size of the deep veins is an important factor when considering the severity of PE. The diameters of the calf veins, the femoral vein, and the common iliac vein are 6–8, 8–10, and 10–12 mm, respectively. On the other hand, the pulmonary artery becomes smaller with distance from the right ventricle. The diameters of the main pulmonary trunk, main pulmonary arteries, and lobar arteries are approximately 25, 15, and 8 mm, respectively. A large thrombus formed in the proximal leg vein may become 8–10 mm in diameter and 30–40 cm in length. This large thrombus can easily pack proximal pulmonary arteries, inducing massive or sub-massive PE.
The pathophysiological effects of massive or sub-massive PE are hypoxemia due to ventilation-perfusion mismatch and right ventricular failure due to reduced net pulmonary arterial vascular beds. The mortality of massive pulmonary embolism is very high: 25% in patients with shock and 65% in patients with cardiopulmonary arrest. Most deaths from massive pulmonary embolism occur in the initial several days, especially within several hours after onset. Therefore, prevention of venous thromboembolism is crucial. Early detection and intervention for massive and sub-massive pulmonary embolism are also important.
The treatment strategy for massive and sub-massive PE consists of three components: i) cardiopulmonary support; ii) anticoagulation to prevent extension and recurrence of PE; and iii) reperfusion of the pulmonary artery by thrombolysis or mechanical removal of emboli. The first simple step in cardiopulmonary support is oxygen administration for perfusion-ventilation mismatch and administration of inotropes for right ventricular failure. If inotropic support fails or the patient develops cardiopulmonary arrest, portable cardiopulmonary support (veno-arterial extracorporeal membrane oxygenator: V-A ECMO) is indicated. Anticoagulant therapy is also important to inhibit the extension of the secondary thrombus in the pulmonary artery. It is also effective for inhibiting the embolization of venous thrombus, which would cause recurrent PE. Heparin should be initiated immediately when PE is suspected as long as the patient has no contraindications to anticoagulation, such as active bleeding from the gastrointestinal tract. Reperfusion therapy is a rational approach to management for occlusion of the major pulmonary arteries. Pharmacological reperfusion using tissue plasminogen activator (t-PA) is effective to improve the hemodynamics of massive or sub-massive PE. The thrombolytic effect of t-PA is as high as 80%; however, a few randomized trials have shown that t-PA improves the prognosis of massive pulmonary embolism. Hemorrhagic complications, especially in aged patients, are major adverse effects of t-PA. Mechanical reperfusion consists of catheter therapy and surgical embolectomy. Catheter therapy was developed by Greenfield in 1969 using a cup-shaped catheter; however, it is not commonly used because of uncertainties about the procedure. Recent catheter interventions include several modalities with or without the use of local thrombolysis. Although local thrombolysis in the pulmonary artery is efficacious, it is difficult in patients with contraindications to thrombolysis, such as patients with stroke or after major surgery. Catheter embolectomy or fragmentation is an alternative to surgical embolectomy, and excellent results for massive and sub-massive PE have been reported. Because patients with massive PE have unstable hemodynamics, use of cardiopulmonary support, or V-A ECMO, is frequently necessary to ensure the safety of the procedure.





