#Industry News
Pulmonary Embolism: Recognizing and Managing a Life-Threatening Condition
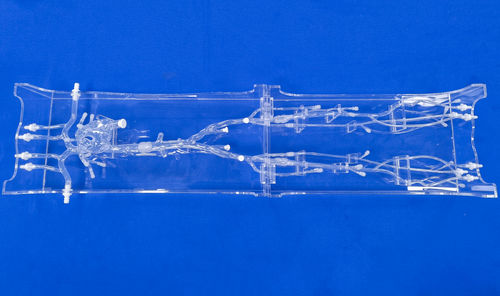
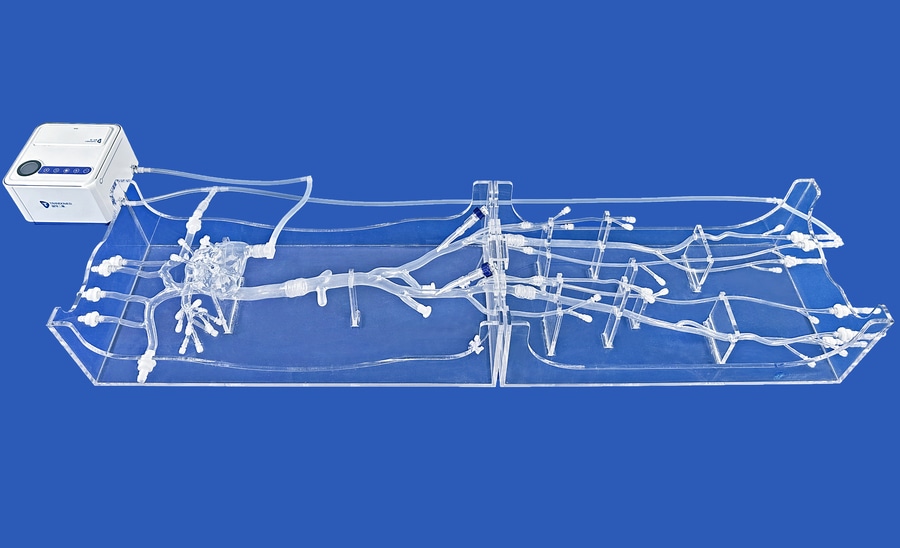
Model:Full Body Veins
Pulmonary embolism (PE) is a critical medical emergency characterized by the sudden blockage of one or more arteries in the lungs, typically caused by blood clots that travel from other parts of the body, most commonly from the deep veins in the legs. This condition poses a significant risk to life and demands prompt recognition and intervention to prevent serious complications. Understanding the causes, symptoms, diagnosis, and treatment of pulmonary embolism is crucial for effective management and improved outcomes.
Causes and Risk Factors:
PE usually arises from deep vein thrombosis (DVT), where blood clots form in the deep veins of the legs and can break loose, traveling through the bloodstream to the lungs. Risk factors for PE include prolonged immobility, surgery, trauma, certain medical conditions like cancer or clotting disorders, smoking, obesity, and hormonal contraception.
Symptoms and Clinical Presentation:
The symptoms of PE can vary widely, making diagnosis challenging. Common signs include sudden onset of chest pain, shortness of breath, rapid heart rate, coughing up blood, and feeling lightheaded or dizzy. However, some individuals may experience atypical symptoms or be asymptomatic, emphasizing the importance of maintaining a high index of suspicion in at-risk patients.
Diagnosis and Evaluation:
Diagnostic tests for PE include imaging studies such as CT pulmonary angiography, ventilation/perfusion (V/Q) scans, and Doppler ultrasound for detecting DVT. Blood tests, such as D-dimer levels, may also be used to assist in diagnosis. A comprehensive evaluation is essential to confirm the presence of PE, determine its severity, and identify any underlying risk factors.
Management and Treatment:
Immediate management of PE involves stabilizing the patient, providing oxygen therapy, and initiating anticoagulant therapy to prevent further clot formation. In cases of hemodynamic instability or large clot burden, interventions like thrombolytic therapy or surgical embolectomy may be necessary. Long-term management typically involves anticoagulant therapy to prevent recurrence and complications.
Prognosis and Prevention:
The prognosis for PE can vary depending on the size of the clot, the patient's overall health, and the timeliness of treatment. Prompt recognition and appropriate management are crucial in improving outcomes and reducing the risk of complications like chronic pulmonary hypertension or recurrent embolism. Preventive measures, including early mobilization after surgery, compression stockings, and anticoagulant therapy in high-risk individuals, are essential in reducing the incidence of PE.
In conclusion, pulmonary embolism represents a serious and potentially life-threatening condition that requires swift recognition, accurate diagnosis, and timely intervention. By understanding the causes, symptoms, and management strategies associated with PE, healthcare providers can effectively address this critical condition, improve patient outcomes, and reduce the burden of this significant cardiovascular emergency.
Introducing the revolutionary Full Body Veins model, a cutting-edge simulator meticulously crafted to emulate the complex intricacies of the cardiovascular system. From the right heart structures to the pulmonary arteries, lower extremity veins, and major vessels extending through the body, this model is encased in a transparent acrylic box, offering a glimpse into the inner workings of the circulatory system. With tailored access points in the femoral vein for interventional tools and customizable connectors, sections of the model can be easily interchanged, catering to a diverse array of educational and research needs with precision and flexibility.
This innovative model transcends traditional boundaries, serving as a dynamic platform for exploration and advancement in cardiovascular medicine. Ideal for the development, testing, and validation of cutting-edge interventional devices targeting the right heart, including guidewires, catheters, balloons, and valve stents, it paves the way for groundbreaking innovations in cardiac care. Moreover, the model facilitates immersive training sessions, live demonstrations, and hands-on practice with interventional devices specific to pulmonary arteries, offering a transformative learning experience. Beyond this, it provides a unique opportunity for mastering surgical techniques related to lower extremity venous occlusions and showcases intricate procedures for pulmonary artery embolism interventions. With its unparalleled design and versatile applications, the Full Body Veins model heralds a new era in cardiovascular education and research, empowering medical professionals to push the boundaries of innovation and excellence in patient care.