#Product Trends
Functional and structural changes in the neuromuscular junction of the diaphragm during premature aging, and methods to slow its degenerative changes
Functional and structural changes in the neuromuscular junction of the diaphragm during premature aging, and methods to slow its degenerative changes
Introduction
The diaphragm neuromuscular junction (NMJ) is a critical connection point between the nervous and muscular systems. It is responsible for transmitting signals from the nervous system to the muscles, triggering muscle contraction. Specifically, the functions of the diaphragm NMJ include the following aspects:
Signal Transmission
When the respiratory center sends a command, motor neurons transmit action potentials along the nerve fibers to the diaphragm NMJ. At this junction, nerve endings release the neurotransmitter acetylcholine (ACh). ACh binds to nicotinic acetylcholine receptors (nAChRs) located on the muscle cell membrane, causing depolarization of the muscle cell membrane, which in turn triggers muscle contraction.
Maintaining Respiration
The diaphragm is one of the primary respiratory muscles. Its contraction and relaxation are essential for the expansion and contraction of the lungs, thereby facilitating the process of breathing. Proper NMJ function ensures the smooth operation of this process.
Adaptive Regulation
The NMJ has a certain degree of plasticity and can adjust its function based on physiological or environmental conditions. For example, during prolonged high-intensity respiratory demands, the NMJ may enhance its signal transmission efficiency to support stronger muscle contractions.
Disease Detection and Diagnosis
The functional state of the NMJ is also an important indicator in assessing certain diseases, such as myasthenia gravis and multiple sclerosis. The pathological processes of these diseases may affect the structure and function of the NMJ, leading to muscle weakness or other symptoms.
Research Objective
Recently, Russian scientist Andrei N. Tsentsevitsky and colleagues conducted a study on the structural and functional changes of the diaphragm NMJ during middle age, publishing their findings in the International Journal of Molecular Sciences. Specifically, the research aimed to understand whether the diaphragm NMJ undergoes changes with aging, especially starting from middle age, how these changes affect neuromuscular communication and diaphragm function, and whether these changes are related to alterations in breathing patterns. By comparing the diaphragm characteristics of young adult and middle-aged mice, the researchers hoped to better understand the mechanisms of age-related diaphragm dysfunction, providing a scientific basis for preventing or treating age-related respiratory problems.
Research Findings
Age-related diaphragm dysfunction often leads to respiratory complications, and NMJ dysfunction may be a key cause of diaphragm weakness in the elderly. While significant structural and functional changes in the diaphragm NMJ of aged rodents have been confirmed, the changes in middle-aged NMJs remain unclear.
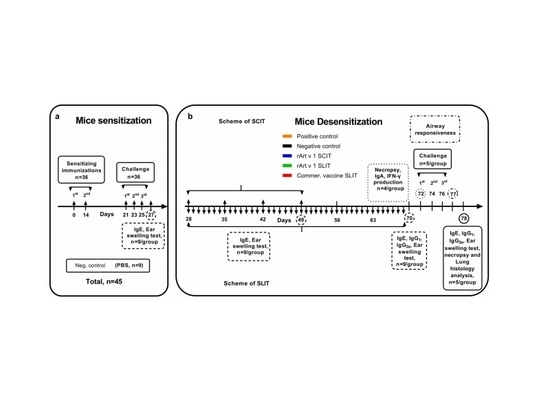
This study compared the diaphragm differences between young adult (3 months old) and middle-aged (12 months old) BALB/c mice using microelectrode recordings, immunofluorescence staining, electron microscopy, muscle mapping analysis, and whole-body plethysmography (WBP) developed by Tow-Int Tech.
The researchers used the Tow-Int Tech WBP to conduct respiratory studies on the 3-month-old and 12-month-old mice, with the graph showing representative recordings. They quantified respiratory rate (A), tidal volume (B), and minute ventilation (C). The charts (D–F) show respiratory dynamic parameters: inspiratory and expiratory times (D), peak inspiratory and expiratory flow rates (E), and mid-tidal expiratory flow rate or EF50 (F). Data are presented as mean ± standard deviation. n = 10 and 11 represent the number of 3-month-old and 12-month-old mice, respectively. p < 0.05 and **p < 0.001 indicate significant differences between groups using the Mann–Whitney U test; "ns" indicates no significant difference.
The study observed an adjustment in breathing patterns in middle-aged mice, marked by an increase in peak inspiratory flow rate and a trend toward higher tidal volume, further confirming enhanced diaphragm activity in these mice. In summary, the study concluded that during early aging, neuromuscular communication in the diaphragm is enhanced due to a strengthening of presynaptic mechanisms, accompanied by an improvement in contraction response.
The researchers' findings not only deepen our understanding of age-related diaphragm dysfunction but also reveal the dynamic changes in the NMJ during aging and their impact on respiratory function. These changes may involve complex molecular mechanisms and signaling pathways, requiring further research for a comprehensive analysis.
Future Research Directions
It is important to note that although middle-aged mice exhibit enhanced diaphragm activity, this enhancement may not be entirely beneficial. Prolonged high-frequency neural activation and increased contraction response could lead to diaphragm fatigue and damage, potentially accelerating the development of diaphragm dysfunction. Therefore, future research should focus on exploring how to balance diaphragm activity and rest through NMJ function modulation to delay or prevent diaphragm dysfunction. The study reveals changes in diaphragm NMJ during early aging and their impact on respiratory function, offering new perspectives and insights into age-related diaphragm dysfunction. Future research will continue to explore unknown areas in this field, with the goal of making greater contributions to human health.
How to Slow Diaphragm Dysfunction
Diaphragm dysfunction can lead to breathing difficulties and reduced exercise tolerance, especially in older adults and those with chronic conditions. Treatment methods typically include the following:
Respiratory Rehabilitation Training
Respiratory muscle training: Specific exercises to strengthen respiratory muscles, such as deep breathing, diaphragmatic breathing, and balloon blowing.
Physical therapy: Professional physical therapists can design personalized training plans to help improve respiratory muscle function.
Pharmacological Treatment:
Bronchodilators: For patients with chronic obstructive pulmonary disease (COPD), bronchodilators can relieve airway constriction and reduce respiratory burden.
Anti-inflammatory drugs:For inflammation-induced breathing difficulties, anti-inflammatory drugs can help alleviate symptoms.
Nutritional Support:
Balanced diet: Adequate protein and vitamin intake promotes muscle repair and regeneration.
Weight management: Maintaining a healthy weight can improve respiratory function, as both excess and insufficient weight may increase respiratory strain.
Oxygen Therapy:
Long-term oxygen therapy: For patients with severe hypoxemia, long-term oxygen therapy can raise blood oxygen levels and reduce breathing difficulties.
Surgical Treatment:
Diaphragm pacemaker: In specific cases, such as diaphragm paralysis due to high spinal cord injury, a diaphragm pacemaker can stimulate diaphragm contraction.
Diaphragm repair surgery: For structural issues like diaphragm hernia, surgical repair may be necessary.
Lifestyle Adjustments:
Smoking cessation: Smoking is a major cause of respiratory diseases, and quitting smoking can significantly improve respiratory function.
Avoiding pollutants: Reduce exposure to air pollutants such as second-hand smoke and industrial emissions.
Regular exercise: Moderate aerobic exercise can strengthen cardiovascular and respiratory function and improve overall health.
Conclusion
Treating diaphragm dysfunction requires a combination of methods, with individualized treatment plans based on the patient's specific situation. Early diagnosis and proactive intervention can effectively improve respiratory function and quality of life. If you or a family member has similar symptoms, it is recommended to consult a healthcare professional for a detailed evaluation and treatment plan.
Tow-Int Tech Whole-Body Plethysmograph (WBP)
Tow-Int Tech has developed a whole-body plethysmograph system (WBP) that allows the measurement of respiratory parameters such as respiratory rate, tidal volume, and airway hyperresponsiveness (AHR) in conscious, freely moving animals. The system avoids the need for invasive procedures like tracheotomy and anesthesia, making the experimental process simpler. It is suitable for respiratory system model animal studies of drug responsiveness, pharmacological, and toxicological research of respiratory medications, especially for high-throughput screening and long-term tracking studies.
Contact us now!
We are committed to making your research easier, more accurate, and more efficient and helping you build confidence in your data! We have provided services for a large number of customers, giving us rich experiences in offering customized, professional solutions according to your needs.